FERTILITY FORWARD: IMPROVING CARE & RESOURCES FOR YOUNG ADULT CANCER CARE IN BC/YUKON
FERTILITY FORWARD: IMPROVING CARE & RESOURCES FOR YOUNG ADULT CANCER CARE IN BC/YUKON
An Anew Research Partnership with Young Adults Navigating Cancer and Care Providers
“You have the shortest window of time to do anything about it.” ~ young adult navigating cancer related fertility care
Every year in Canada, nearly 8,300 young adults ages 15-39 are diagnosed with cancer meaning nearly 1 young adult diagnosed every 65 minutes. For these individuals, a cancer diagnosis can be especially devastating for those hoping to have children either in the near or long term. In fact, the impact of cancer treatment on fertility is among the most pressing concerns identified by young adults navigating cancer. Accessing timely fertility preservation services and effective information and support with which to make critical decisions is not always easy in BC/Yukon.
Opportunity to Improve
The Anew Research Collaborative, based at Royal Roads University, and led by Dr. Cheryl Heykoop, Michael Smith Health Research BC Scholar, who herself experienced cancer as a young adult, is partnering with young adults with cancer navigating cancer, and care providers at BC Cancer, BC Children’s Hospital, Vancouver General Hospital and Yukon Hospitals, to gain a clear understanding of the gaps in fertility services, information and support in BC/Yukon – including determining how these gaps can be effectively addressed collaboratively going forward. This work is supported by the Canadian Partnership Against Cancer.
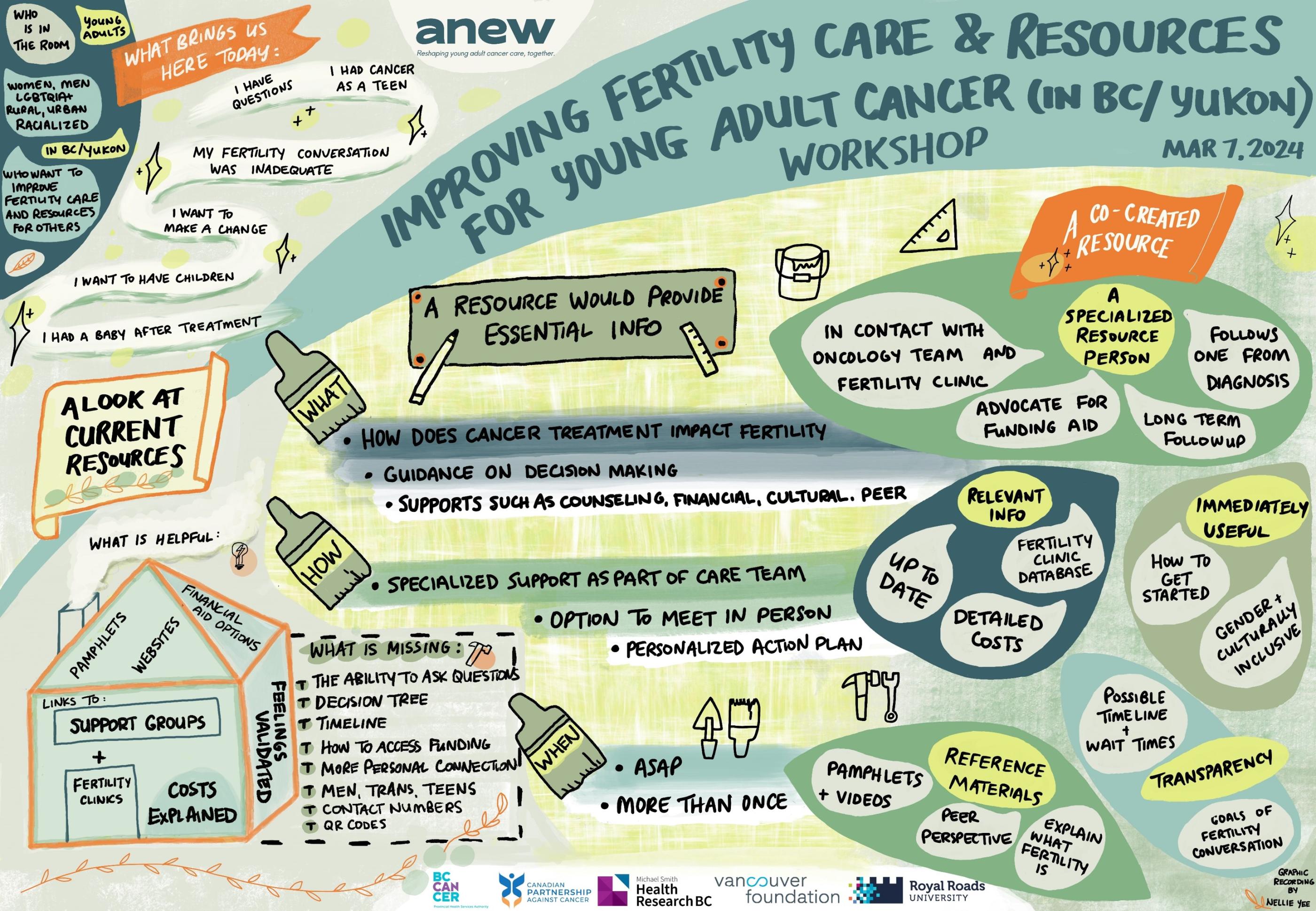
Anew, a patient-oriented, participatory action-based research program dedicated to reshaping young adult cancer care together with young adults and care providers, facilitated the first in a series of interactive workshops with young adults on this challenge earlier this spring. Eighteen young adults with cancer experience from BC/Yukon gathered for an evening via Zoom engaging in discussions and generative, creative exercises to co-design a strategy to inform development of effective resources to support decisions regarding cancer related fertility preservation.
Learnings Summary
Here are the key themes shared by young adults at this workshop –
- Young adults want the complete picture – up front.
Effective fertility resources provide all the information needed to make fertility preserving decisions including details on procedures such as in-vitro fertilization, cryopreservation and sperm storage and potential changes depending on one’s stage of cancer and treatment. Inclusion of perspectives from young adults who have experienced fertility preservation was highlighted as very important.
- Be transparent re: cost – or not.
All agreed that fertility preservation is costly. Some participants expressed the importance of resources clearly articulating the financial implications of each procedure including secondary costs associated. Others thought differently, however, citing that knowing the cost could be a deterrent when there may be options to offset costs.
- Make informational resources cross-provincial and multi-model.
Rural and remote versus urban is another important consideration to accessing fertility services. As such participants recommended that resources reflect the sometimes-transient nature of accessing support and treatment and provide contact details for fertility clinics throughout the region. The use of QR codes was also recommended to increase access to information.
- Resources need to be inclusive and representative.
Participants emphasized that resources need to represent different intersectional identities i.e., an image of a white woman with a ‘baby bump’ holding the hand of a white man does not represent the experiences of other gender identities or races. They stressed that resources should incorporate images and language that are gender and culture inclusive.
Moving Forward
Upcoming engagements are now being planned with groups of young adults from underrepresented groups and efforts are beginning, too, to connect with clinicians and related care providers to better understand their cancer related fertility practices including sharing insights from young adults to date and gathering their thoughts on tangible opportunities for improvement. A collaboratively developed fertility preserving care pathway and an outline for effective resources are the intended outcomes of this work in the coming months. Register for updates via anewresearch.ca